Cancer doesn’t always have to mean a death sentence.
As the matter of fact, more than half of the cancers we know today are preventable through awareness. Oftentimes, what’s needed is knowledge of their symptoms for early detection of the disease.
This is why cancer awareness months are especially important!
This month of September is dedicated to a certain type of cancer affecting women—ovarian cancer. Consultant Medical Oncologist from Beacon Hospital, Dr Azura Rozila Ahmad chats with Motherhood Story to help shed light on ovarian cancer and how it comes to affect women.
Q1: What is ovarian cancer and how does it affect women?
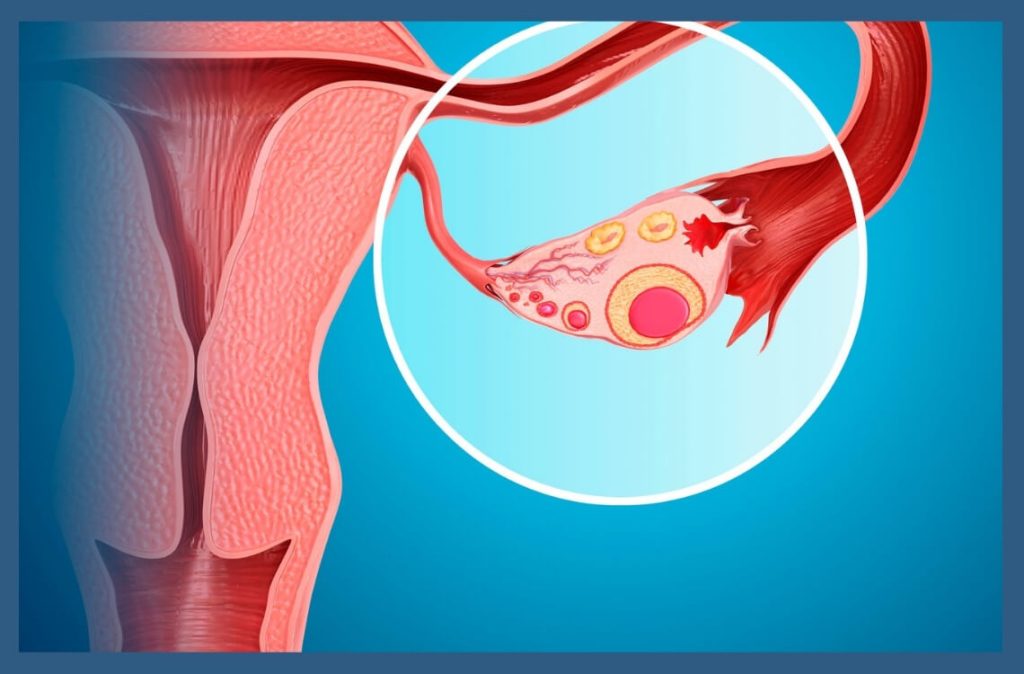
Dr. Azura: It is a cancerous growth of cells originating anywhere in the ovaries or the fallopian tubes. The cells multiply uncontrollably and may spread out to invade surrounding structures within the pelvis, abdominal cavity, or beyond.
There are usually two ovaries in the female reproductive system, one on each side of the uterus. The ovaries, about the size of an almond, are responsible for the production of eggs (ova) as well as the female hormones; oestrogen and progesterone.
Ovarian cancer can arise from different types of cells within the ovaries and sometimes from outside the ovary. More than 70% of ovarian cancers can develop from the surface of the ovaries (epithelial carcinomas); while other forms of ovarian cancer can come from cells that produce eggs (known as germ cell tumours) or in connective tissue (called stromal cell tumours). Occasionally, cancers cells from other organs, usually from around the pelvis and abdomen can also land on the ovary and form metastatic disease.
Q2: How common is ovarian cancer among Malaysians? Who is most likely to get ovarian cancer?
Dr. Azura: According to the Malaysian National Cancer Registry of 2012-2016, cancer of the ovary is ranked tenth as the commonest cancer overall. It is ranked fourth amongst females and is the highest killer among all female cancers. The group of women with the highest number of cases reported in Malaysia occur in women who are already in menopause (age mid-60s). However, it can occasionally affect younger women. For example, germ cell tumour is more common in younger women under the age of 30.
Q3: Is ovarian cancer linked to any other forms of cancer?
Dr. Azura: Notably, there are a few conditions where different cancers occurring in the family can be linked to the possibility of an inherited form of ovarian cancer:
Hereditary breast and ovarian cancer syndrome (HBOC)
Dr. Azura: This is caused by inherited mutations in the BRCA1 and BRCA2 genes, as well as possibly some other genes yet to be discovered. This syndrome is associated with an increased risk of breast, ovarian, fallopian tube, and primary peritoneal cancers. Other cancers, such as pancreatic cancer and prostate cancer, are also at increased risk.
Some families have mutations in the BRCA1/2 gene and these women have significant risks of developing breast and ovarian cancers.
If you think there is a familial pattern, speak to a doctor for a referral for a genetic assessment.
Q4: Are there causes to ovarian cancer? Can genetics or Human papillomavirus (HPV) play a role?
Dr. Azura: Although the exact cause of ovarian cancer is unknown, doctors have identified risk factors that may increase the risk of the disease. Some of which are:
- Increase age (most important).
- Having a first-degree relative with ovarian cancer (mother, sister, or daughter).
- Not having children.
- Having a first child at a later age (first pregnancy age > 35 years old).
- Beginning menstruation at a young age.
- Experiencing menopause later in life.
- Having uterine, breast, or large intestine (colon) cancer, or having a family member who has had one of these cancers.
- Being overweight.
- Smoking.
- Lack of exercise.
- Exposure to asbestos.
As mentioned earlier, occasionally ovarian cancer can be inherited. A small proportion of ovarian cancers are caused by genetic changes inherited from your parents or grandparents.
Specific inherited genes such as BRCA1 and BRCA2 are two genes that can increase the risk of ovarian cancer quite significantly. It is important you find out the risk of cancers in your family and talk to your doctor if you suspect there is a familial pattern.
Q5: What are the early warning signs of ovarian cancer?
Dr. Azura: Ovarian cancer symptoms can be vague and unfortunately can be mistaken as a non-threatening condition causing delaying in diagnosis. In the early stages of the disease, there may be no symptoms or even minimal complaints even.
Common symptoms may be as follows:
- Bloating of the abdomen.
- Pelvic or abdominal discomfort.
- Unexpected mass in your abdomen or pelvis.
- Having difficulty eating or feeling full quickly.
- Urinary frequency or urgency.
- Backache.
- Fatigue.
- Pain while having sex.
- Constipation or stomach upset.
- Changes in a woman’s menstrual cycle.
- Weight loss.
- Unexplained fatigue.
- Shortness of breath.
Pay attention to your body and understand what is common for you. Consult a doctor if your symptoms are unusual, more frequent, persisting (e.g. for more than two weeks), worsening, or out of the ordinary. Don’t rely on Google only as they are intended for a general guide that may not be applicable for you.
Q6: How does one receive their diagnosis?
Dr. Azura: If you do have symptoms that warrant further assessment, your doctor may perform a blood test, physical examination including a pelvic exam in addition to radiological tests (usually abdominal or transvaginal ultrasound initially).
If cancer is suspected, you may need a biopsy, usually performed by the gynaecology surgeon. A suitable method will be used to obtain a tissue sample. The sample is then examined in the pathology laboratory to confirm the diagnosis. Sometimes, you may go straight to surgery if the diagnosis is very likely and the disease is operable.
Commonly, following a cancer diagnosis, additional tests such as CT scan and MRI scan may be performed to confirm and determine where the cancer has spread and to decide if surgery is possible.
Q7: What do you think are the challenges that come with the diagnosis?
Dr. Azura: Diagnosis is challenging because of many factors. Ovarian cancer is known as the “silent killer” due to only minimal or little symptoms in early stages.
Also, many with symptoms are only diagnosed when already in advanced stages. Due to its vague presentation which can also mimic other conditions, it can delay diagnosis as it would be assumed and treated for another condition first. Furthermore, screening tests can be unreliable, unlike with breast cancer.
We need to raise more awareness on this form of cancer as its symptoms are easily misdiagnosed or dismissed.
Due to the highest occurrence of ovarian cancer amongst women above the age of 50, many may have competing medical conditions, which need to be factored in when planning optimal treatment.
In general, treatment planning is complex, requiring coordinated efforts between different doctors including surgeons and oncologists. If surgery is indicated, an aggressive surgery is preferred as it may provide better outcomes and should be performed by a specialised surgeon. To reduce the potential risk of recurrence, chemotherapy is commonly recommended to most patients after surgery. Chemotherapy can cause hair loss and may not be favourable for patients. All these factors can seem very daunting for many women and they need support while on treatment.
When the disease is inoperable due to the extent of spread, chemotherapy may be given first with consideration for surgery later after a few cycles of treatment.
Q8: What does the road to recovery look like? What sort of treatments will a patient have to undergo?
Dr. Azura: Treatment is typically based on the type of ovarian cancer, its stage, and any special circumstances. The majority of women with ovarian cancer will undergo surgery to remove the tumour. Depending on the type of ovarian cancer and how advanced it is, you may require substantial treatment before or after surgery or both.
Ovarian cancer is typically treated with a combination of surgery and chemotherapy. Surgery is the primary step, with the aim of removing as much of the tumour as possible, a process known as debulking. Chemotherapy is mainly used after surgery because most women are diagnosed after the disease has spread.
Some patients can be treated with chemotherapy alone depending on the subtype and patient’s condition.
Q9: How likely is it for ovarian cancer to come back?
Dr. Azura: Risk of recurrence depends on its stage. Even for early-stage diseases like Stage 1C, the risk is still significant and as a result, many women may be offered chemotherapy after surgery.
Every case will be weighed against risk and benefit. Discuss with your oncologist what is right for you.
For advanced cancers that cannot be cured, typically women will undergo multiple courses of drug treatment which in this modern era may be personalised according to their specific cancer mutation detected in their cancer.
Q10: What can our readers do to reduce their risks of ovarian cancer?
Dr. Azura: Although ovarian cancer cannot be totally prevented, there are ways to reduce the risk. Increasing awareness and education about cancer will help you navigate your personal health and seek medical attention early.
Some suggestions are:
- Obtain and maintain a healthy weight throughout adult life.
- Maintain physical activity and limit time spent sitting or lying down.
- Maintain a healthy eating pattern that includes plenty of fruits, vegetables, and whole grains while limiting or eliminating red and processed meats, sugary drinks and highly processed foods.
- It is best not to consume alcohol. If you do drink, limit yourself to one drink per day for women or two drinks per day for men.
- Know your family history and if there is a possibility of any genetic risk, ask your doctor where you can assess your risk to adopt the right strategy for you.
- Go for medical check-ups regularly and get your concerns addressed if you have any worrisome symptoms.
Source: Dr Azura Rozila Ahmad, Consultant Medical Oncologist, Beacon Hospital
Disclaimer: The information provided in this article is for informational purposes only and should not be considered as medical advice from Motherhood. For any health-related concerns, it is advisable to consult with a qualified healthcare professional or medical practitioner.
For more insightful stories and fun recipes, stay tuned to Motherhood Story!