Lysosomal Storage Diseases, or LSDs is a rare genetic disorder that manifests itself as early as childhood. If left untreated, it can have a significant impact on young lives.
Now, as parents, this may be the first time you’re hearing about this. While uncommon, it’s still important to learn as much as we can about conditions and illnesses that can affect our little ones.
We had a chat with Dr Ngu Lock Hock, Department Head of Genetics, Clinical Geneticist and Paediatrician, Hospital Kuala Lumpur, to talk about lysosomal storage disorders, also commonly known as LSDs.
Q1: What exactly are lysosomal storage disorders (LSDs), and how do they occur?
Lysosomal storage diseases, or LSDs, are a group of about 50 different conditions, different diseases. They are grouped together as a lysosomal disease. All of these are genetic conditions.
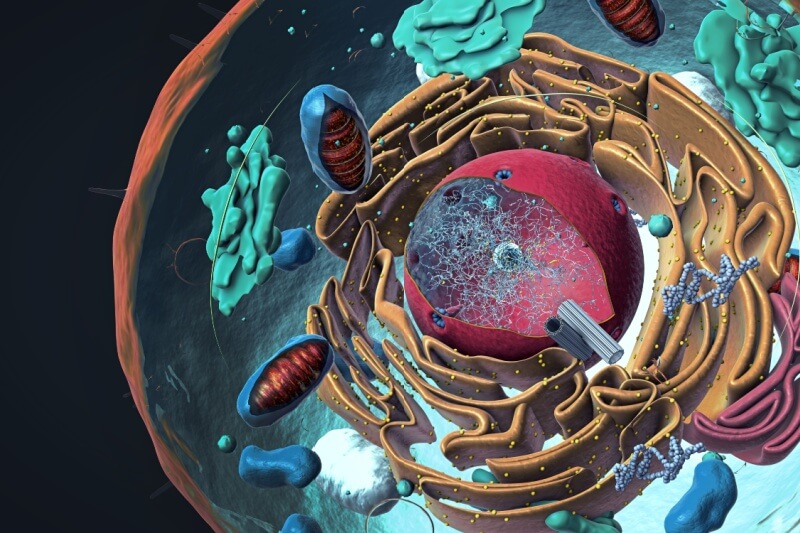
If we look at our cell, it consists of many such organelles or side units. You have a nucleus which stores all the genetic material, and one of the components of our cell is lysosome.
Inside this lysosome, you have various kinds of enzymes. So, lysosome functions like a recycling centre for our cell.
Imagine our cell components, like the cell membrane and other parts; over time, they get torn and worn.
So, all of these materials, the old materials, will be sent to the lysosome.
Inside the lysosome, there are these various enzymes; they work together to process it. Those that can be reused will be recycled. Those that cannot be reused will be disposed of as waste.
The lysosome is actually like a waste disposal system for your body. These enzymes are made in our cells based on the instructions in our genes.
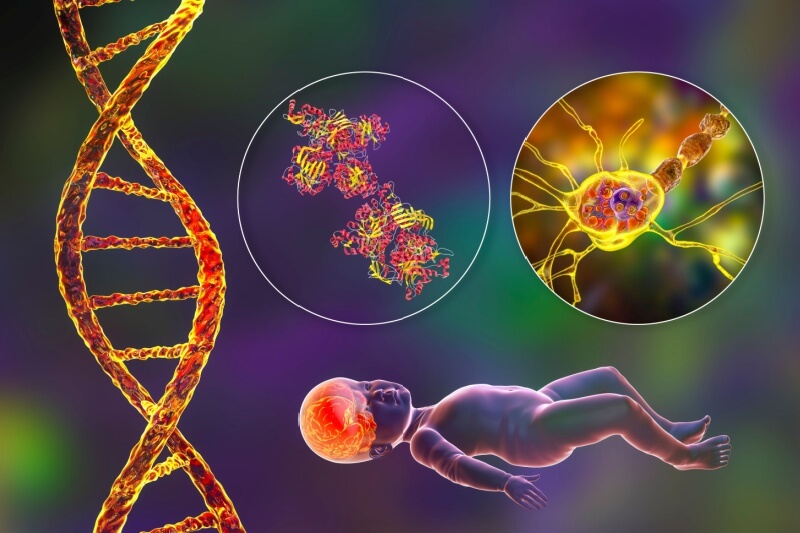
If there’s some mistake in the gene, the cells don’t get the information to make the correct enzymes for the lysosome. Because of this, certain waste products and waste material in the cell cannot be broken down.
So, these waste products, they will accumulate in this lysosome, in the cells, in the organs, and they build up in our body later on. This can happen in our cells as well.
Q2: How common is this condition?
Each individual that I see, they are rare. But because you’re talking about more than 50 different conditions here, cumulatively, they’re probably not that uncommon. Maybe 1 in 250,000 people, to 1 in 500,000 people.
Some that I see are more common in my personal clinical practice will be Pompe disease, Gaucher disease, and mucopolysaccharidoses.
I know these are all difficult words to pronounce. You can call it in short term, MPS.
Even with MPS, there are many types. There is Type 1, there is Type 2, and there is Type 3.
Q3: Let’s talk about the symptoms. If a child has LSD, what might parents or carers notice about their child who has this?
Obviously, this is not an easy job. Not only for the parents, sometimes even for the healthcare professionals, because we are talking about a rare disease here.
It can overlap with many other conditions. The clinical signs and symptoms can differ from one disease to another.
So, first I will talk about Pompe disease.
For Pompe disease, there is an accumulation of the waste material that accumulates here, which is glycogen.
The tissue and the organ that are most affected are the muscles. So, it can be your heart muscle; it can be your lean muscle.
Even in Pompe disease, you have early-onset and the later-onset time.
In the early onset we are talking about, it can affect babies that are less than two years old.
So, usually, because it affects the muscle, it will result in what I call a floppy baby.
And they don’t achieve their normal developmental milestones. They will have delays in walking and delays in all these motor developments.
And their heart muscles are also affected. Their heart muscles get enlarged. Because of this, they often have recurrent chest infections.
This can also affect adolescents and adults, where, because of muscle involvement, they’ll have problems climbing stairs or taking part in sports activities. Or sometimes because of muscle weakness their spine gets bent. We call this scoliosis.
So, these are some of the manifestations we can see in LSD, in particular, Pompe disease.
Of course, for other diseases like MPS, their management is slightly different.
So, in MPS, all the babies are born normal. Normal physically.
But the red flag will be, they’ll get a runny nose that does not resolve even after getting treatment. They frequently get ear infections, like middle ear effusion.
Sometimes they get a hernia, which is not something that’s common in babies. Hernia usually occurs in adults, especially. They can have hernias on both sides, right and left. This is very unusual, so that is another red flag.
The other thing will be because all this waste material accumulates in their body, under their skin.
So, their facial features will change with time, what we call ‘coarse’ in medical terms.
They can also deposit in the liver and in the spleen, so they get organ enlargement. The liver gets enlarged, and the spleen gets enlarged. These are a few other red flags that I think parents can look out for.
But it’s not necessarily that if you have the disease that presents symptoms at a very young age, it means that people develop it later on in life. It depends on the severity of the genetic mutation.
So, they will manifest early – in early childhood. If their genetic mutation is less and milder, they will develop the disease in adulthood.
Q4: How can parents differentiate between normal variations in development and something that is more serious, for example, like LSD?
Obviously, this is not an easy task. If you have noticed one of these red flags, the next step is to consult a doctor, such as a general practitioner or a paediatrician, so they can do some examinations.
Based on the clinical findings, there are certain tests that can be done to confirm whether this is LSD. So, basically, there are three types of tests.
One, we look for the biomarker. So, like in MPS, we can check the child’s or person’s urine to see any accumulation of these abnormal waste methods.
Second, we can check the lysosomal enzyme. So, all these lysosomal diseases are due to a certain defect or deficiency in the enzyme. We can check all these enzymes through the blood sample.
Thirdly, of course, we can check the genes to see whether there was a mistake. So, these are the sort of tests that can be considered when somebody has certain signs or symptoms that may suggest that it’s LSD.
If the general practitioner or paediatrician are unsure, they can always refer to the Genetics Department in HKL. We can guide them through all this process.
Q5: What happens if these conditions go undiagnosed?
All these LSDs, they are what you call progressive diseases. Your cellular waste accumulates more and more every day.
Obviously, with time, there are more complications that may develop to the extent that they may affect the lifespan of a person – causing a lot of inconvenience and disability.
So, early diagnosis is important. Because among 50 different types of LSDs, about 10 different types have available treatments.
This treatment is called enzyme replacement therapy. This means that you replace the missing enzyme through intravenous infusion.
Of course, the treatment is more effective if we start it early, at the early stage of the disease. This is another important reason why we want to diagnose, detect this condition early.
Even in some countries, they have introduced what are called newborn screening programmes. For every newborn, they will check their blood to see whether they’ll be affected by one of these conditions. So, the treatment can be started as soon as possible.
Because that way, you’re able to get rid of the toxins. But of course, for some LSDs, at the moment, there are no effective treatments.
But science is always progressing, so the possibility of other treatments like gene therapy or some other form of pharmaceutical therapy probably will be found in the near future.
And I think it really shows that the importance of awareness, as early diagnosis can make a huge difference in somebody’s clinical health.
Q6: What kind of support do you think parents can have? Is there some sort of support system for parents who have children that are going through this very rare disease?
This disease has a huge impact. Not only for the individual but the parents too. So, they obviously require some help from many people.
We do have some patient support groups locally. For example, the Malaysian Lysosomal Disease Association. They can offer assistance or support to the patient and their family to get them through this tough moment.
The Malaysian Lysosomal Diseases Association is a dedicated organisation committed to supporting families affected by lysosomal storage disorders.
Parents can learn more about their work and access valuable information at www.mymlda.com or follow their updates and initiatives at facebook.com/MLDA.
Disclaimer: The information provided in this article is for informational purposes only and should not be considered as medical advice from Motherhood. For any health-related concerns, it is advisable to consult with a qualified healthcare professional or medical practitioner.
For more insightful stories and fun recipes, stay tuned to Motherhood Story!